The human spinal column is a complex structure made up of many integrated tissues, bones, muscles, and nerves. Helping to cushion the weight between the vertebrae are a series or cartilage discs that act as shock absorbers and help you move, bend and twist comfortably. As time goes by, the natural aging process, and other factors can cause these discs to wear down.
Degenerative disc disease is a term used to describe this process. It is an inevitable reality that everyone’s spinal discs degenerate with age. Though for some people degenerative disc disease can be so severe that it causes increasing discomfort and can lead to other medical complications.
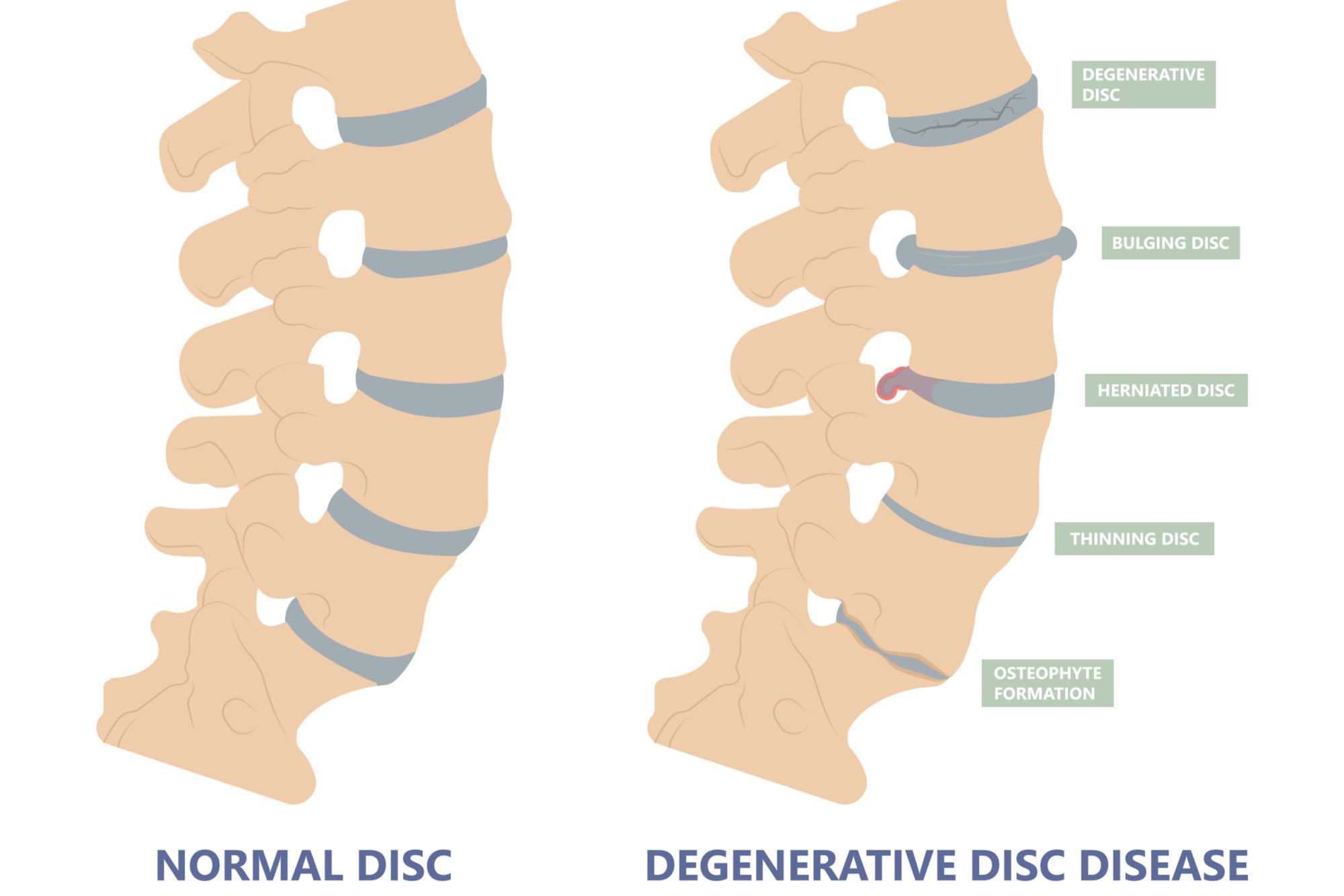
As the vertebral discs start to wear away, the bone surfaces can start to rub together. This sort of grinding friction can cause pain and other complications such as:
- Adult-onset scoliosis
- One or more herniated or ruptured discs
- A narrowing of the spinal column known as Spinal stenosis
- Spondylolisthesis that causes the vertebrae to move in and out of their natural position
When Does Disc Degeneration Start?
Most people will have some degree of disk degeneration starts by the age 40. Though less than 5% of people have noticeable symptoms. It can lead to back pain in about 5% of adults.
What Increases The Risk For Degenerative Disc Disease?
Degenerative disc disease is most common in older adults. Some factors increase your risk of developing degenerative disc disease, including:
- Acute back injuries
- Taking a hard fall
- Obesity
- Smoking
- Working a physically labor intensive job
It’s also worth noting that women are more likely to experience degenerative disc disease symptoms.
Common Symptoms Of Degenerative Disc Disease
Many people start to experience the early stages of degenerative disc disease with gradually neck pain and back pain. At first the discomfort might come and go, lasting longer each time it returns. As degenerative disc disease progresses you might notice additional symptoms such as:
- Numbness or tingling in your arms
- Numbness or tingling in your legs
- Pain that radiates down to your buttocks and lower back
- Discomfort that worsens with sitting, bending or lifting
What causes degenerative disk disease?
Changes In The Vertebral Discs
As you age the discs in your back start to grow through subtle changes. This includes things like:
Loss of Moisture
Each of your vertebral discs has a soft core with water retained inside. As you age this core naturally loses some water. This causes the disks to get thinner, while also reducing their shock absorption ability.
Cracks & Tears
At the same time, the membrane of the vertebral discs can also become fragile and vulnerable. Even seemingly minor injuries can cause small cracks in your spinal disks. Unfortunately, this typically occurs near highly sensitive nerves.
This means that these cracks and tears can be very painful, even when they are minor. If the outer wall of your spinal disk cracks open, your disk may bulge out of place. Also known as a “Herniated Disc” it has a high likelihood of compressing a spinal nerve.
How Is Degenerative Disc Disease Diagnosed?
Diagnosing degenerative disc disease starts with your physician evaluating your symptoms. This typically includes questions like:
- When did the pain start?
- Where is the pain most common?
- Which activities and motions cause the most pain?
- Which activities and motions decrease the pain?
- Have you recently had an injury or accident that led to pain?
- Are you experiencing symptoms, such as tingling or numbness?
- How far can you walk?
Your physician might also take some imaging scans such as X-ray, CT or MRI to help them better evaluate the state and alignment of your discs. This is usually done in conjunction with a physical exam to evaluate your condition. This includes some of the following tests for
Nerve function, which involves using a basic reflex hammer to check your reactions and evaluate the risk of compressed nerves.
Pain levels, which involves touching or pressing on specific areas of your back to measure your pain levels.
Strength testing, to assess potential. muscle weakness or shrinking (atrophy) could mean you have nerve damage or degenerated discs.
How Is Degenerative Disc Disease Treated?
With most cases of degenerative disc disease, your physician will likely recommend noninvasive treatment options first. This might include things like
Physical therapy sessions that focus on strengthening and stretching exercises.
Medications such as nonsteroidal anti-inflammatory drugs, muscle relaxers or steroids.
Direct steroid injections near your spinal nerves, or discs to help reduce inflammation and manage discomfort.
Radiofrequency neurotomy, which uses electric currents to burn sensory nerves to help prevent pain signals from reaching your brain.
Degenerative Disk Disease Surgery
Surgery is rarely needed in mild to moderate cases of degenerative disc disease. Though it might be the final option that your physician recommends if multiple nonsurgical treatments have failed to deliver the results you need to maintain your mobility and quality of life.
If surgery is indicated, your physician might recommend one of the following procedures.
Discectomy
This surgical procedure involves removing part of a spinal disk to relieve pressure on your nerves.
Foraminotomy
This technique calls for expanding the opening for your nerve roots by carefully removing small sections of bone and other related tissues.
Laminectomy
This is an open surgical procedure that involves removing a small portion of bone from your lower spinal region known as the Lamina.
Osteophyte Removal
This is a minimally invasive surgical treatment that essentially removes bone spurs known as osteophytes from the vertebrae surrounding compromised disks.
Spinal fusion
This surgery involves your surgeon permanently connecting two or more vertebrae to improve stability.
Preventing Degenerative Disc Disease
While you can never 100% prevent degenerative disc disease, there are some things that you can do to slow the progression of spinal degeneration through lifestyle changes. This includes things like:
- Losing weight and maintaining a healthy body weight.
- Quitting smoking.
- Exercising regularly
Performing physical therapy exercises to improve strength and flexibility.
Other Conditions That Can Occur With Degenerative Disc Disease
Most degenerative disc disease sufferers can effectively manage their pain with nonsurgical and at-home treatments to manage pain long-term. Though even after surgery, you will need to continue exercising and stretching to keep your back strong and healthy. Some patient’s experience additional complications associated with degenerative disc disease such as:
- Osteoarthritis
- Scoliosis
- Spinal stenosis
- Spondylolisthesis
- Spondylolysis