The human shoulder is a compound joint with an impressive range of motion. It transfers force from the arms to the torso of your body in complex ways that play a critical role in your overall quality of life. However, injuries, repetitive use, and even the natural aging process can all put you at risk of a wide range of shoulder problems. Not the least of which is a condition known as Frozen Shoulder.
Frozen shoulder is a term that is often used to describe the gradual loss of movement or reduced range of motion in the shoulder’s glenohumeral joint. This large ball and socket joint includes the humeral head or the upper arm as well as the glenoid socket of the shoulder girdle itself. Anytime the shoulder is frozen, the movement in the joint is limited or perhaps severely impaired.
Common Causes of Frozen Shoulder
While many shoulder conditions, injuries, and joint diseases cause some degree of pain and loss of range of motion, a frozen shoulder is often associated with inflammation, swelling, pain, and general irritation in a wide range of the tissues surrounding the ball and socket of the shoulder joint.
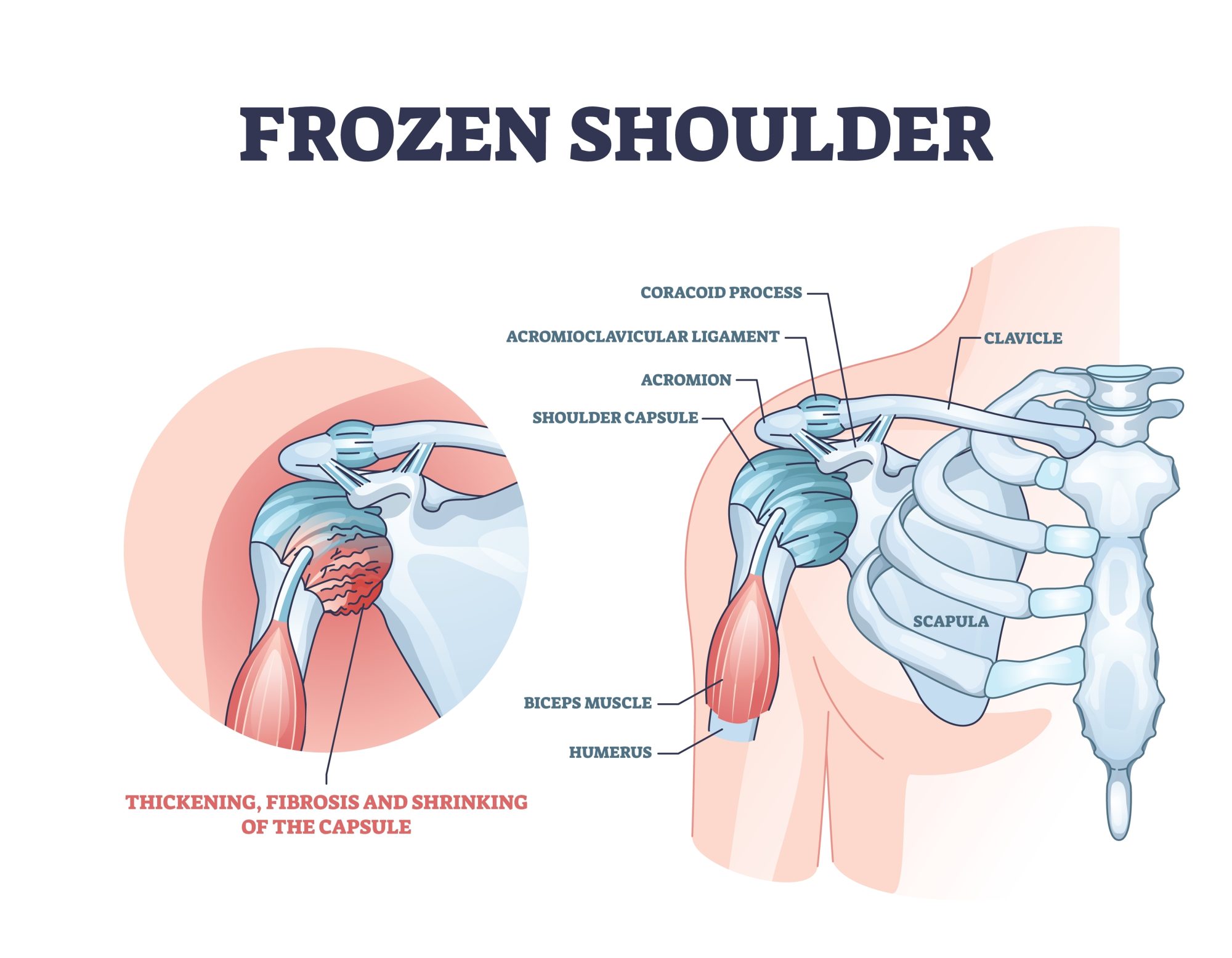
The tissues around the shoulder joint, holding all the structures together is known as the capsule. It has structural folds that can expand and contract when the arm moves into various positions in the natural range of motion.
In the case of a frozen shoulder, this capsule becomes inflamed to the point that scarring begins to develop in the soft tissues and connective tissues. This type of scar formation is known as adhesions.
Over time the capsule’s folds become scarred with adhesions, which causes all the structures to tighten. As it progresses the shoulder’s range of motion becomes increasingly restricted to the point that moving the joint becomes painful. This condition is called “Adhesive Scarring Capsulitis, which notes the inflammation of the capsule’s various tissue structures.
Despite extensive orthopedic research in this area, the cause of frozen shoulder is still not 100% known. Though things like immobilization of the shoulder, which might occur after an arm injury, seem to increase the risk of developing a frozen shoulder. At the same time, there are conditions such as rotator cuff tendinitis or bursitis, that can also cause the shoulder joint to become frozen due to chronic inflammation in the capsule tissues.
Diagnosing Frozen Shoulder
Accurately diagnosing frozen shoulder starts with your physician taking a complete history to understand all the possible contributing factors. This is then followed up by a physical examination to test the range of motion and discomfort.
If your frozen shoulder symptoms are significant, your physician will likely refer you for imaging diagnostics such as X-rays or an MRI. This will help to rule out other potential causes of a painful shoulder or limited shoulder motion. It can also help to detect comorbidities of the shoulder joint such as arthritis, calcium deposits, or damage caused by a previously undiagnosed shoulder injury.
How Is Frozen Shoulder Treated?
Treatment of frozen shoulder often requires a two-fold approach. This starts with improving the overall range of motion in the shoulder joint as well as effectively decreasing pain.
Improving Range of Motion With Frozen Shoulder
With a lot of cases of frozen shoulder, improving the range of motion typically involves prolonged physical therapy. This starts with an experienced physical therapist moving the affected arm in a clinical setting to stretch the capsule.
These sessions also help teach the patient a range of home exercises that they can do to further improve the range of motion in their frozen shoulder. These stretching exercises might include the use of a wand or overhead pulley.
Your physical therapist might also use ice, heat, ultrasound, or some type of electrical stimulation therapy. This will help loosen scar tissue in the capsule, while also serving to improve blood flow to the affected tissues. Your physical therapist will demonstrate a stretching program that you should do at least once or twice a day.
Decreasing the Pain of Frozen Shoulder
When it comes to the pain management aspect of a frozen shoulder a lot of physicians start with anti-inflammatory medications such as aspirin, ibuprofen, Naprosyn, and Aleve. In a more significant case pain medications such as Tylenol or narcotic pain medication might be prescribed to decrease the pain after therapy. They might be taken in limited applications to help with sleep at night.
In some frozen shoulder cases, steroid injections in the joint or the nearby bursa might be required to reduce inflammation and boost the body’s natural healing process. This might also include taking oral steroids such as prednisone in conjunction with the injection.
Physical Therapy & Rehab For Frozen Shoulder
A lot of frozen shoulder cases call for supervised physical therapy. This is a combination of clinical sessions, as well as at-home stretching exercises that can last from one to six weeks. Over time the frequency of visits can range from one to three times per week.
During the physical therapy process, you will need to actively engage in home exercises and stretching throughout the healing process to maximize results and make progress toward improving the overall range of motion in the affected shoulder.
A lot of the stretching exercises should be done at home at least once or twice. Fortunately, most cases of frozen shoulder tend to resolve themselves with time and consistent compliance with the prescribed treatment program.
Just keep in mind that the therapeutic process can sometimes take as much as six to nine months for some patients. The internal rotation motion, where you move your hand to the back pocket or up the middle of your back is often the type of motion that takes the longest to fully restore.
When Is Surgery Needed To Treat Frozen Shoulder?
Surgical treatment is usually the last resort for treating a chronic case of frozen shoulder. If the non-invasive techniques and physical therapy don’t improve the range of motion in your shoulder and significantly decrease pain, then surgery might be required.
Frozen shoulder alteration surgery is typically performed on an outpatient basis and requires a general or local anesthetic. During the surgical procedure, the surgeon might manipulate the shoulder in the operating room to remove some of the scar tissue.
In many of these cases, an arthroscope with an attached camera is placed into the shoulder capsule via a small puncture-type incision. The camera guides other instruments to directly cut or release the capsular adhesions.
Afterward, a lot of patients begin physical therapy the same day as the manipulation or the following day. This helps maintain the newly released range of motion, as well as reduces the chances of new post-operative surgical scarring developing.