The health of your feet is easy to overlook until there is a problem. When something like Plantar Fasciitis affects one of your feet, the discomfort and outright pain can hamper your quality of life, not to mention your overall mobility.
What Is Plantar Fasciitis?
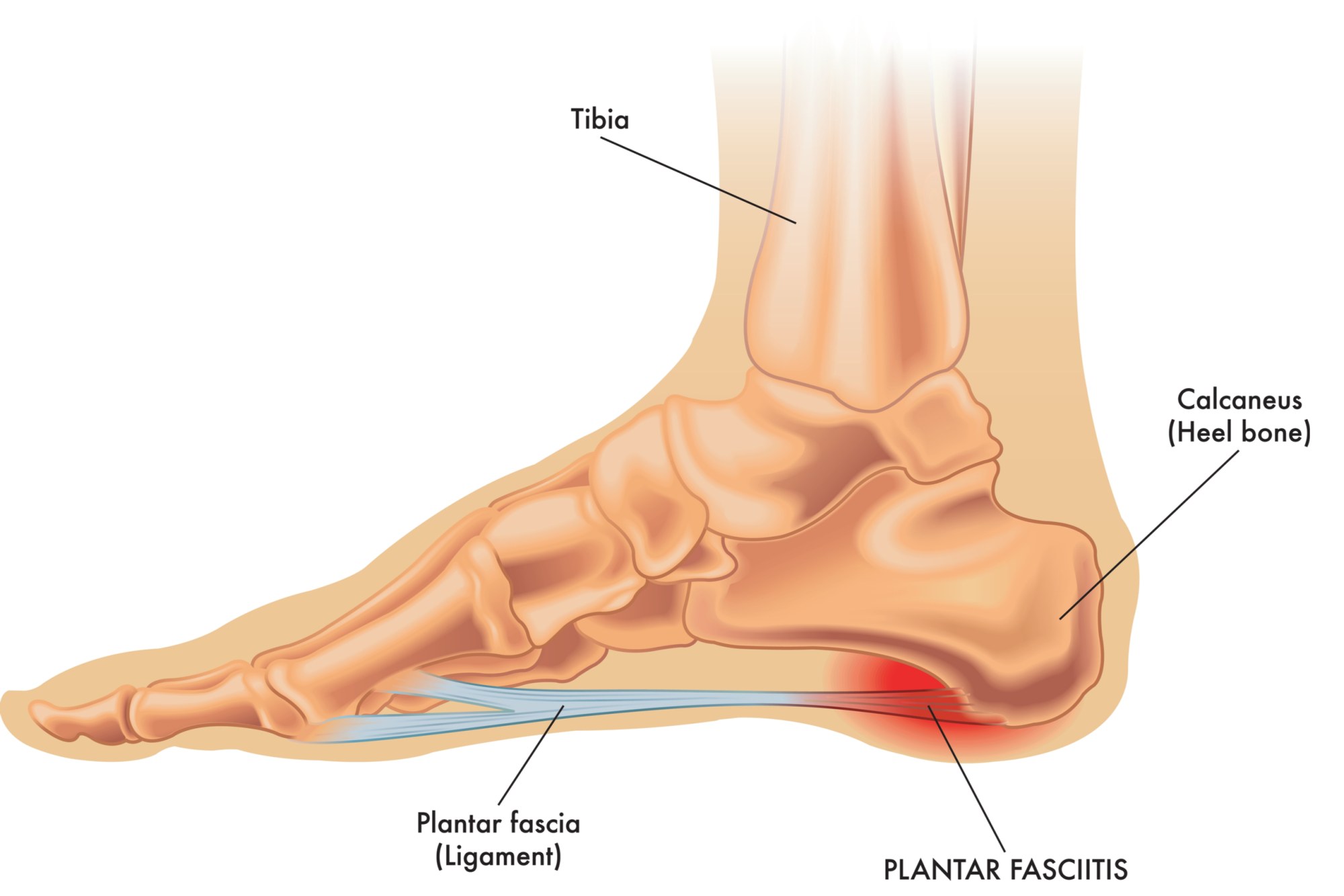
The plantar fascia in each of your feet is a thick, weblike ligament that serves a functional purpose in firmly connecting the structures in the front of your foot to your heel. It also serves as a sort of shock absorber as it helps to support the arch of your foot. In this way, it plays an important role in helping you walk, jog, run and jump.
Unfortunately, plantar fasciitis happens to be one of the more common orthopedic complaints, as the plantar fascia ligaments tend to experience a lot of wear and tear. It’s also possible for high pressure on your feet to damage or essentially tear some or all of these ligaments. Though even without a physical tear inflammation in the plantar fascia can cause significant pain and stiffness in the heel of your foot.
What Are The Symptoms Of Plantar Fasciitis?
One of the earliest symptoms of plantar fasciitis is a recurring pain in the bottom of the heel which can sometimes spread to the bottom of the mid-foot area. It typically affects a single foot, though it can sometimes affect both feet.
Unless it is related to a recent injury the pain and discomfort from plantar fasciitis tend to develop gradually over time. This pain can be dull or in a severe case sharp. Some people experience a burning or ache on the bottom of the foot extending outward from the heel.
Most plantar fasciitis sufferers note that the pain and discomfort are typically worse in the morning when they first step out of bed. Some notice that they will feel increasing discomfort if they’ve been sitting or lying down for an extended period of time. Climbing stairs can be very difficult due to heel stiffness.
What Causes Plantar Fasciitis?
Active adults between the ages of 40 to 70 years old tend to be the highest risk group for developing plantar fasciitis. It’s worth noting that it is slightly more common in women than men. Especially in women who are pregnant, who sometimes experience bouts of plantar fasciitis inflammation during the later stages of pregnancy.
You’re at a greater risk of developing plantar fasciitis if you’re overweight or obese. This is due to the increased pressure on your plantar fascia ligaments, especially if you have sudden weight gain.
Long-distance runners and other sports that call for a great deal of running can also place you at a higher, risk for developing plantar fascia problems. At the same time, individuals with very active professions that involve being on your feet for a long period of time, such as working in a factory or being a restaurant server.
Adults with certain structural foot issues such as high arches or very flat feet, may develop plantar fasciitis. An overly tight Achilles tendon in the back of the leg can affect also increase your risk of developing plantar fasciitis.
Of course, all of these risk factors are also increased by wearing poor shoes that have overly soft soles and poor arch support can also result in plantar fasciitis.
How Is Plantar Fasciitis Diagnosed?
The first step in diagnosing plantar fasciitis involves your physician performing a routine physical exam of your feet to check for tenderness. Be sure to let them know the exact location of the pain. It’s important to make sure that the pain isn’t the result of a different foot problem.
During the exam, your physician will likely ask you to flex your foot while they push on the plantar fascia to see if the pain gets worse as you flex and better as you point your toe. Your physician might also note if you have mild redness or swelling.
The diagnostic exam will then evaluate the strength of the muscles in and around the foot as well as the health of your nerves. This includes things like checking your:
- Reflexes
- Lower body muscle tone
- Your basic sense of touch
- General coordination and balance
In some cases, your physician might also refer you for diagnostic imaging. An X-ray or an MRI might be necessary to check that nothing else is causing your heel pain, such as a bone fracture.
How Is Plantar Fasciitis Treated?
For a mile case of plantar fasciitis, where the damage to the connective tissue is minimal or the symptoms are related to modest inflammation, home treatment measures such as rest, icing, or using braces might be sufficient to abate symptoms. This might also include prescription anti-inflammatory medication.
If your symptoms don’t improve, or the discomfort and inflammation are more significant, an injection of a corticosteroid directly into the damaged section of the ligament can help. Your physician can usually do this in their office. This might involve using an ultrasound device to help determine the best placement for the injection.
With a lot of cases of plantar fasciitis, physical therapy plays an important role in the treatment strategy. This is designed to help stretch your plantar fascia as well as other lower body connective tissues such as the Achilles tendons.
If your discomfort and pain persist your physician might recommend a treatment known as “Extracorporeal Shock Wave Therapy. This involves using sound waves to bombard your heel to stimulate healing within the ligament.
Surgery For Plantar Fasciitis
Surgery is one treatment of last resort for most plantar fasciitis cases and is only indicated if the pain is severe or lasts more than 6 to 12 months.
Known as “Plantar Fascia Release” it involves a surgeon partially detaching the plantar fascia from your heel bone. This acts to reduce the tension but weakens the arch of the foot, and full function may be lost.
If you have a hard time flexing your feet even after consistent stretching, your doctor may recommend gastrocnemius recession. This surgery involves lengthening the calf muscle to increase ankle motion and release stress on the plantar fascia.